What kind of improvement are you looking for?
Organization-Wide vs. Department-Specific
Take a look at how we can help you reach your improvement goals:
Improve RN Engagement
%
Overall Average Improvement for All Categories

*Results were measured from the start of project to Submission (and later successfully designated)
Improve Quality (NSIs)
%
Overall Average Improvement for All Categories
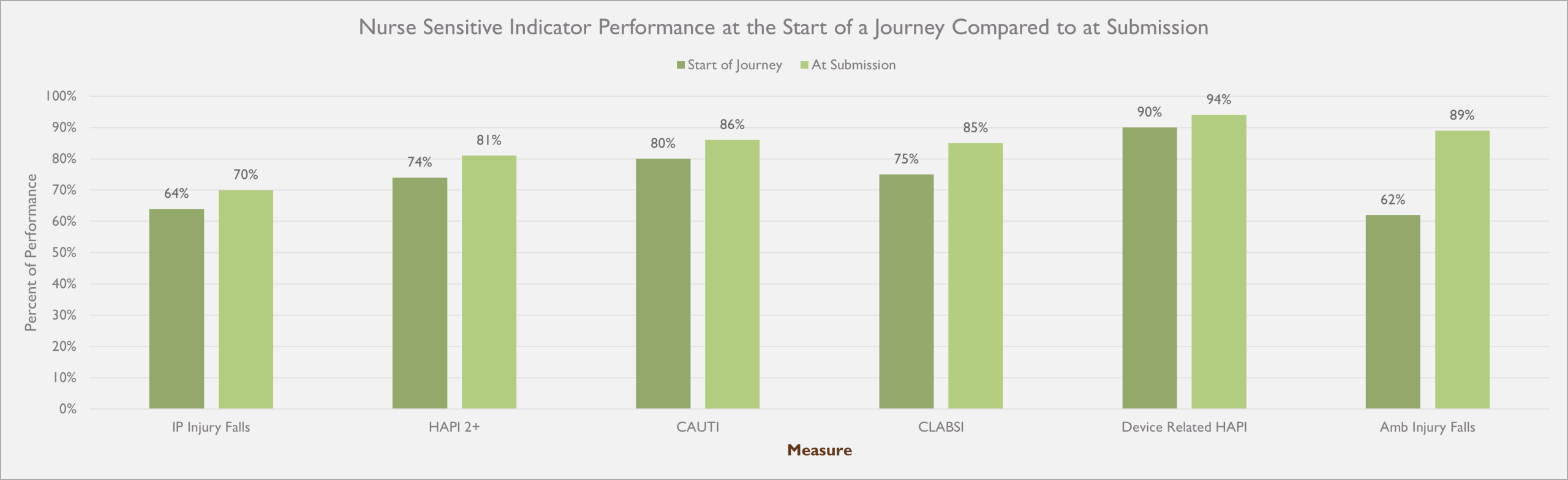
*Results were measured from the start of project to Submission (and later successfully designated)
**HealthLinx’ costs were easily covered by the reduction of avoidable costs from improved NSIs.
Improve Patient Experience
%
INPATIENT
Overall Average Improvement for All Categories
%
AMBULATORY
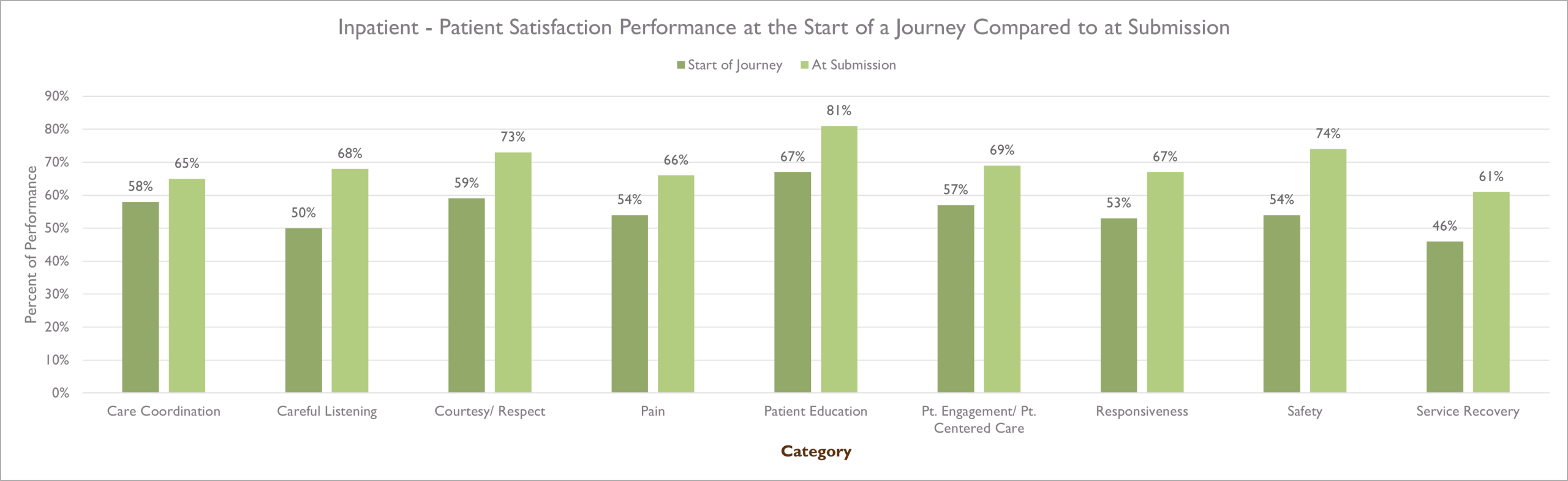

*Results were measured from the start of project to Submission (and later successfully designated)
**HealthLinx’ costs were easily covered by the reduction of avoidable costs from improved NSIs.
Improve Care Management
Pursue Model Performance In Care Management
- <10% readmission rate
- LOS within 0.85 of expected stay
- Avoidable Emergency Department Visits <5%
- Screenings >90% of patients for SDOH
- >95% of high risk patients received follow-up call within 48 hours of discharge
- Multi-Disciplinary rounds completed by 11 AM
DIRECTOR OF CARE MANAGEMENT
- 300+ Beds
- Community Hospital
——————————————————
- High LOS resulting in ED throughput issues
——————————————————
- $3 Million in Financial Benefit
- LOS reduced from 5.1 to 4.39
Improve Critical Care
Pursue Model Performance In Critical Care
- 50% or greater CCRN certifications of eligible RNs
- Near zero incidents of CLABSI, HAPI, Falls, & VAEs
- Near zero mislabeled specimens
- Near zero medication errors
- Standardized Mortality Ratio below 0.8
- RN Turnover rate less than 10%
- Unplanned return to Critical Care Unit within 48 hours of discharge/transfer less than 3%
DIRECTOR OF CRITICAL CARE
- 400+ Beds
- Academic Hospital
——————————————————
- Position open 8 months with Stretch Coverage
——————————————————
- $1.7 Million in Financial Benefit
- RN Turnover Reduced
- CAUTI and Falls Reduced
Improve Cardiovascular Services
Pursue Model Performance In CV Services
- <2% CABG risk adjusted mortality rate
- <4% Heart Failure risk adjusted mortality rate
- <1.2% Cath PCI risk adjusted mortality rate
- <10% 30 Day Readmission Rate (All Cause)
- Procedural Complication Rates <1% (Stroke, bleeding, vascular complications)
- On-Time Case Starts >95%
- Patient Satisfaction Scores >90%
- Participation in national registries (NCDR, STS, GWTG, SVS, CathPCI®)
DIRECTOR OF CARDIOVASCULAR CATH LAB
- 250+ Beds
- Flagship Hospital of a System
——————————————————
- 10-month vacancy needing quality metrics improved
——————————————————
- $913,000 in Financial Benefit
- Staffing Model Revised
- Data sharing with physician teams
- Supply Cost per Unit of Service reduced
- Achieved in 8 months
Improve Emergency Department
Pursue Model Performance In the Emergency Department
- Door to Provider time of <10 minutes
- LOS for Discharged Patients <120 minutes
- LWBS rate <2%
- ED boarding time <90 minutes
- Top Box score in patient satisfaction >90%
- Readmission rate (30 day return to ED) <5%
- >90% adherence to the sepsis bundle within 3 hours
- Time to analgesia for long bone fractures <30 minutes
- Door to needle for Stroke (TPA administration) <30 minutes
- Door to balloon (STEMI) <90 minutes
- >85% ED RN Satisfaction
- <10% RN turnover rate
DIRECTOR OF EMERGENCY DEPT.
- Level II Trauma
- Community Hospital
——————————————————
- LOS & LWBS were high, experiencing capacity issues
——————————————————
- $3.6 Million in Financial Benefit
- Immediate bedding implmented
- Rapid triage protocols initiated
- LWBS reduced
Improve Med-Surg
Pursue Model Performance In Med-Surg
- CAUTI <0.75 per 1000 catheter days
- CLABSI <0.5 per 1000 line days
- C Diff infection rate <3 per 10,000 patient days
- Fall rate w/ injury <0.5 per 1,000 patient days
- HAPI <1% incidence rate
- Readmission rate for general med-surg patients <8%
- Avg LOS 3.5 days or less
- RN satisfaction >85%
- RN Turnover <10% annually
- Patient Satisfaction overall hospital rating (9 or 10) >85%
- Early Discharge Rate: >30% of patients discharged before noon
- >98% compliance with medication reconciliation at admission and discharge
MED-SURG NURSE MANAGER
- 500 Beds
- 30-Bed Med-Surg Unit
——————————————————
- High capacity- stays full. Struggles with Turnover and Quality outcomes.
——————————————————
- $185,000 in Financial Benefit
- RN Turnover reduced
- Falls and C-Diff Reduced
- Achieved in 8 months
Improve Oncology
Pursue Model Performance In Oncology
- 30 day mortality rate <3% for inpatient hospital admissions
- CLABSI <1 per 1,000 line days
- CAUTI <1 per 1,000 catheter days
- HACs <1% incidents in oncology patients
- Unplanned 30 day readmission rate <5% from chemotherapy & post surgical patients
- >90% of patients start within evidenced based timeframes
- >90% of patients report adequate pain control
- LOS for oncology inpatients <4.5 days for non-complicated cases
MED-SURG ONCOLOGY NURSE MANAGER
- 700+ Beds
- Community, Teaching Hospital
——————————————————
- Turnover, Employee Engagement, Falls and Patient Satisfaction
——————————————————
- $1.6 Million in Financial Benefit
- Turnover Reduced
- Rounding & hardwiring Best Practices increased Patient Experience
- Achieved in 211 Days
Improve Perioperative Services
Pursue Model Performance In Perioperative Services
- Surgical Site Infection Rate <0.5% for clean cases, <1% for all cases
- Unplanned return to OR within 30 days <1.5%
- Postoperative Mortality Rate (30 day all cause) <1% for elective procedures
- Anesthesia related complications <0.2% of cases
- DVT/PE rate <0.3% with appropriate prophylaxis
- Medication Error Rate <0.05%
- FCOTs >90%
- OR Turnover time for general cases, <30 minutes, Ortho/Neuro <35 minutes
- Same day cancellation rate <2%
- OR Block Utilization >85%
- Day of Surgery Admit to Incision Time <60 minutes
- 95% of scheduled cases finish within projected time
- OR utilization rate >75% during prime hours
- Patient Satisfaction >90th percentile
- >50% of hospital margin from surgical services
DIRECTOR OF PERIOPERATIVE SERVICES
- 90+ Beds
- Small, Suburban Hospital
——————————————————
- Increase volume, decrease costs, and implement best practices
——————————————————
- $6 Million in Financial Benefit
- 36.8% increase in Billable Minutes
- 68.5% decrease in Labor Cost
- 32% decrease in Turnover Time
Interested in Organization-Wide Improvement?
Interested in Department-Specific Improvement?
Improvement & Data Resources
How a Nursing Excellence Journey Impacts RN Engagement, Nurse Sensitive indicators, and Patient Satisfaction
The culture created by a Nursing Excellence Journey leads to better patient quality outcomes, increased Patient Satisfaction results, and improved nurse engagement.
Data, Data Everywhere – How to Correlate Data Effectively to Positively Impact Performance
To minimize confusion, correlate data points to provide insight into why adverse events take place. This insight leads to more specific actionable interventions that can positively impact performance.
Med-Surg Transitional Leadership – Video Case Study #3082
A Transitional Leadership Project in a large Med-Surg unit reduced falls, implemented LPNs and reduced Agency use saving $1 Million+